Traumatic Brain Injuries cause over 1 million people in the United States to present to emergency care facilities each year, or over 10 million people per year in the world [1-3]. Traumatic injuries may include blunt trauma, penetrating trauma, blast wave trauma, or rotational trauma. The mechanical forces of trauma can cause temporary shock to neural networks as well as more permanent damage to the tissue and axonal connections between neurons. In addition, bleeding, swelling, and stretching of tissues can worsen cellular death and cause various forms of excitotoxic injury and secondary messenger cascades that can cause delayed cell death. Thus treatments of severe traumatic brain injury generally include surgical decompression, hemostasis and removal of blood, relief of pressure on the brain through drainage of cerebrospinal fluid, and general supportive care to ensure good control of oxygenation and blood pressure. Patients may suffer mild traumatic injuries, which include temporary mild cognitive impairment, confusion, headache, blurred vision, slurred speech, attention deficits, memory loss, or other forms of neural dysfunction, or severe injuries, which tend to result in various forms of permanent neural damage, coma, minimally conscious state, vegetative state, or death by neurologic criteria. Repeated injuries can result in the dangerous “second impact syndrome” (SIS) or, over longer periods of time, may result in chronic traumatic encephalopathy (CTE), which is characterized by atrophy and neurodegeneration in the brain and clinical signs of dementia, depression, memory loss, and other behavioral changes. Even low grades of traumatic brain injury can cause long-term problems such as headaches, depression, fatigue, sleep disorders, mood changes, seizures, restlessness, loss of coordination, memory loss, confusion, and other symptoms similar to post-traumatic stress disorder. Ongoing treatments may include medicines to treat a patient’s specific symptoms, such as antidepressants and anticonvulsants, as well as rehabilitation and physical therapy, speech therapy, psychiatric help, and social support. Neural tissue engineering and stem cell therapy hold the most potential for people who have suffered localized areas of severe neural tissue damage that have the potential to be restored with cellular support and discrete reconstruction of neural networks [4-5].
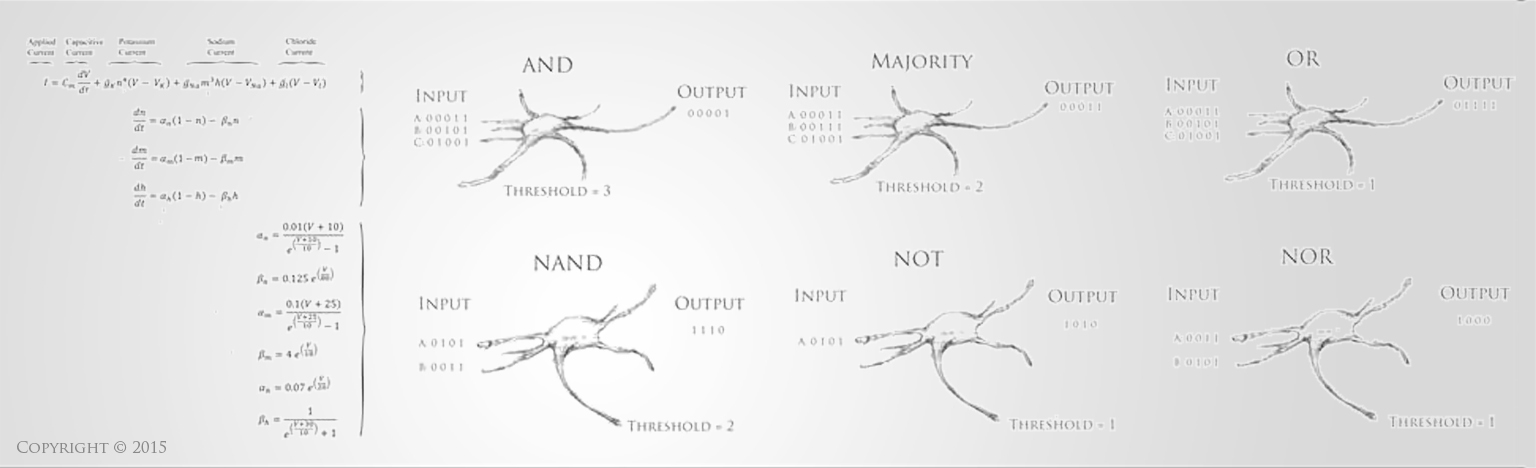
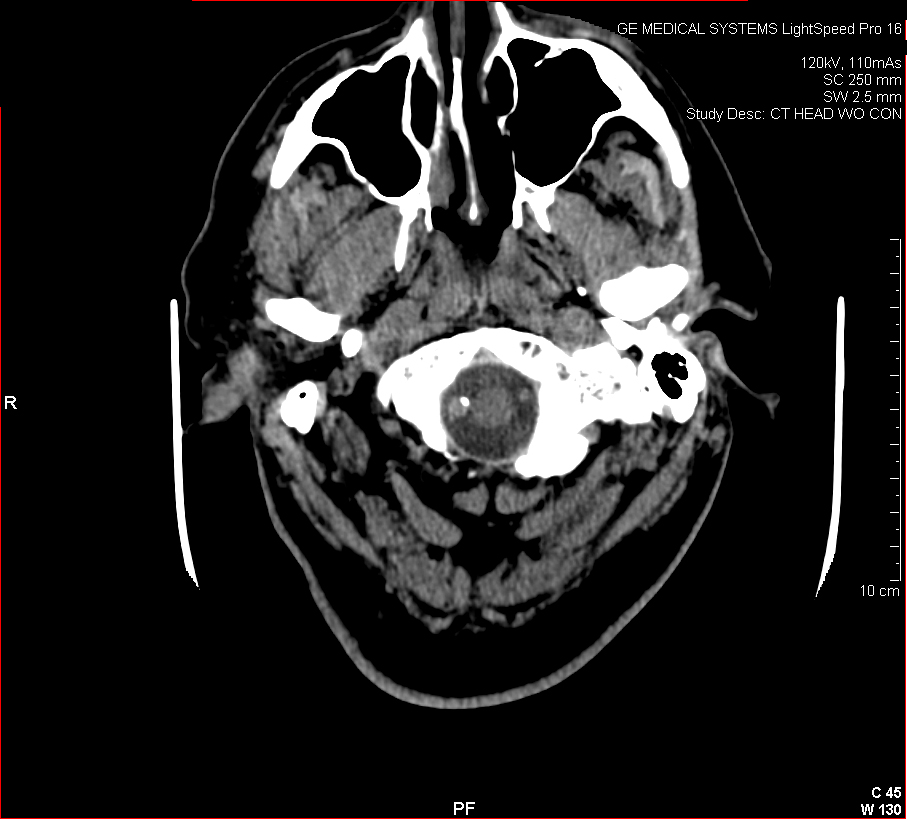
The images below show a CT scan of a traumatic head and neck injury, with a dissection of the right vertebral artery (left image) and a large stroke and intracerebral hemorrhage (ICH) with midline shift on the right side of the brain and a contusion overlying the skull (right image). (Images courtesy of Dr. McMurtrey)
-------------------
References:
1) Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 21(5), 375, 2006.
2) Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. J Head Trauma Rehabil. 25(2), 72, 2010. (Erratum 25(3), 224, 2010.)
3) Gustavsson A, et al. CDBE 2010 Study Group. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 21(10), 718, 2011. (Erratum 22(3), 237, 2012.)
4) McMurtrey RJ. Patterned and Functionalized Nanofiber Scaffolds in 3-Dimensional Hydrogel Constructs Enhance Neurite Outgrowth and Directional Control. J. Neural Eng. 11 (2014) 066009
5) McMurtrey RJ. Novel Advancements in Three-Dimensional Neural Tissue Engineering and Regenerative Medicine. Neural Regeneration Research. 2015 Mar; 10(3).
-------------------
Copyright © 2014 Institute of Neural Regeneration & Tissue Engineering. All Rights Reserved.
Back to Education
|